In a dramatic turnaround that highlights the complex intersection of healthcare policy and individual need, British Columbia’s Ministry of Health has reversed its decision regarding life-sustaining medication for seven-year-old Lily Elson. The young Vancouver Island resident, who suffers from an ultra-rare and potentially fatal genetic disorder, had previously been denied provincial coverage for a drug treatment costing approximately $400,000 annually.
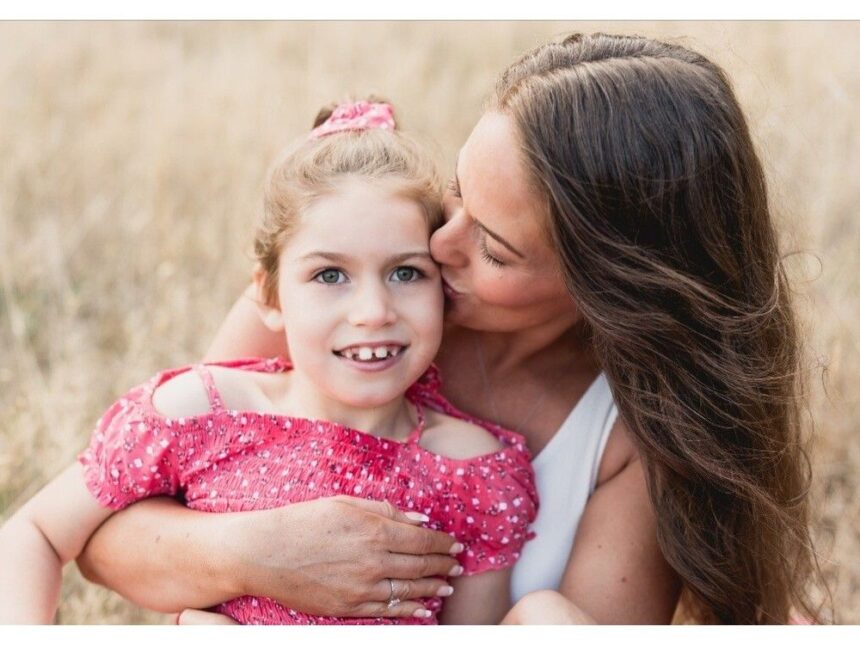
The ministry’s initial refusal to fund Trikafta, a medication that Lily’s doctors insist is essential for treating her specific form of cystic fibrosis, sparked widespread public outcry and intense advocacy from her family. “We’ve been fighting this battle for months while watching our daughter’s health deteriorate,” said Lily’s mother, Sarah Elson. “The constant worry that your child might not receive the medication they desperately need creates an unimaginable burden.”
Cystic fibrosis affects approximately 4,300 Canadians, causing the production of thick mucus that can severely damage the lungs and digestive system. However, Lily’s case is further complicated by a rare genetic mutation that affects fewer than 20 people across the country. This rarity had placed her in a troubling healthcare gap, where standard approval protocols for drug funding often fail to accommodate exceptional circumstances.
British Columbia’s Special Authority program, which governs exceptional drug coverage, initially determined that Lily’s specific genetic variant didn’t meet the established criteria for Trikafta funding. The ministry had maintained that there was insufficient evidence that the medication would be effective for her particular mutation, despite her medical team’s professional assessment and preliminary positive response to the treatment.
Health Minister Adrian Dix confirmed the reversal in a statement Tuesday, acknowledging that “in exceptional circumstances like Lily’s, we must find ways to work within our system to meet unique healthcare needs.” The decision comes after mounting pressure from medical professionals, patient advocacy groups, and political representatives across party lines.
Dr. Mark Chilvers, Lily’s respirologist at BC Children’s Hospital, expressed relief at the decision. “We’re seeing promising responses to Trikafta in patients with various genetic profiles. For children like Lily, early intervention can significantly improve long-term outcomes and quality of life.”
The case has illuminated broader systemic challenges in how provincial healthcare systems address rare diseases. Cystic Fibrosis Canada has been advocating for more flexible approaches to drug approval and funding that consider the unique circumstances of ultra-rare conditions. “When dealing with extremely rare mutations, traditional evidence thresholds are nearly impossible to meet through conventional clinical trials,” noted Kim Steele, Director of Government Relations at CF Canada.
The Elson family’s struggle parallels similar battles occurring across Canada’s healthcare landscape, where patients with rare conditions often find themselves caught between rigid funding frameworks and the astronomical costs of specialized medications. While pharmaceutical innovation continues to develop targeted therapies for previously untreatable conditions, healthcare systems worldwide are grappling with sustainability concerns and equitable access models.
Financial analysts note that the rising costs of specialty medications present significant challenges to provincial health budgets. “The tension between providing patient access to breakthrough therapies and maintaining fiscal responsibility is increasingly difficult to navigate,” explains healthcare economist Dr. Emily Parker. “Each exceptional case approval creates precedent questions that policymakers must carefully consider.”
For the Elson family, the immediate relief overshadows these broader systemic questions. “We can finally focus on Lily’s health instead of fighting bureaucracy,” Sarah Elson remarked. “But we remain concerned for other families facing similar situations who don’t have the resources or public support to advocate so effectively.”
As Lily begins her treatment regimen with secure funding, her case raises critical questions about Canada’s approach to rare disease treatment. How can our healthcare system evolve to balance fiscal responsibility with compassionate care for those with ultra-rare conditions, and what reforms might create more transparent, consistent pathways for exceptional cases without requiring families to wage public battles for access to life-changing medications?