The sudden closure of Port Alice Health Centre this past weekend has sparked renewed concerns about healthcare accessibility in rural Vancouver Island communities. Residents of the small northern village found themselves without local emergency medical services from Friday evening until Monday morning — a troubling development in a community where the nearest hospital is over an hour’s drive away.
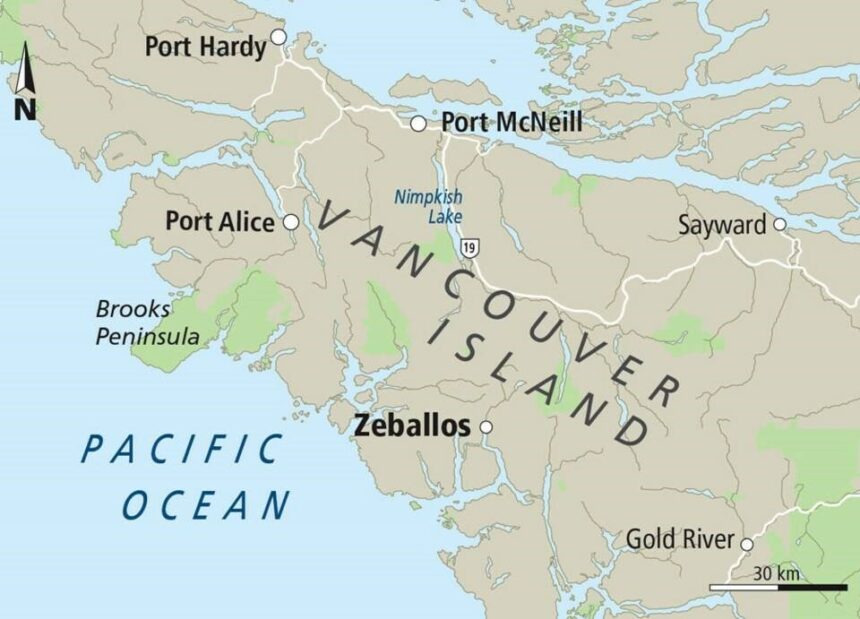
Island Health confirmed the temporary shutdown was due to an “unexpected nursing shortage,” forcing patients requiring urgent care to make the 85-kilometer journey to Port Hardy Hospital or the 50-kilometer trip to Port McNeill Hospital. For elderly residents and those with limited transportation options, this situation created a potentially dangerous gap in essential services.
“This isn’t just an inconvenience — it’s a matter of life and death for some of our most vulnerable community members,” said Maria Connors, a Port Alice resident and healthcare advocate. “When you’re having a medical emergency, that hour-long drive can be the difference between recovery and tragedy.”
The closure highlights the ongoing healthcare staffing challenges plaguing many rural Canadian communities. According to data from the Canadian Institute for Health Information, rural areas consistently struggle with healthcare professional recruitment and retention, with nursing shortages becoming increasingly common across British Columbia’s remote regions.
Port Alice, with its aging population of approximately 700 residents, has been particularly vulnerable to these healthcare disruptions. The health centre, which provides emergency services, primary care, and limited acute care, is considered a lifeline for the community.
Local officials have expressed frustration with what they describe as a pattern of service interruptions. “We’ve been raising alarms about staffing issues for years,” noted Village Councillor Jeff Barnes. “Each time there’s a closure, we’re told it’s temporary, but the underlying problems aren’t being addressed with the urgency they deserve.”
Island Health has stated they are “actively working to recruit additional nursing staff” and implementing “creative solutions” to address the ongoing staffing challenges. However, many healthcare experts point out that broader systemic changes are needed to solve rural healthcare shortages.
“The solution isn’t just hiring more nurses for Port Alice — it’s creating sustainable working conditions that will make rural practice attractive long-term,” explained Dr. Evelyn Chen, a healthcare policy researcher at the University of Victoria. “This means competitive compensation, professional development opportunities, adequate housing, and meaningful integration into the community.”
As Port Alice’s health centre reopened Monday morning, residents expressed relief but remain concerned about future closures. Community leaders are now calling for emergency contingency plans, including potential helicopter medical services during facility closures and guaranteed accommodation support for patients needing to travel to other communities for care.
The situation in Port Alice reflects a wider Canadian healthcare crisis that continues to disproportionately impact rural and remote communities. As policy makers grapple with solutions, residents are left wondering: at what point does “temporary” service disruption become an accepted norm, and what will it take for equal healthcare access to become a reality for all Canadians, regardless of their postal code?