In the bustling corridors of British Columbia’s healthcare facilities, a quiet revolution is taking place. Physicians are now spending more time making eye contact with patients and less time typing notes, thanks to artificial intelligence tools that are transforming how frontline healthcare operates across the province.
At Surrey Memorial Hospital’s busy emergency department, Dr. Adam Lund demonstrates how voice-recognition AI transcribes his patient interactions in real-time, generating comprehensive medical notes without requiring his attention on a keyboard. “The difference is remarkable,” Dr. Lund explains. “I can maintain a human connection with my patients while the technology handles the documentation burden that typically consumes up to 50% of clinical time.”
This technological advancement comes as part of a broader provincial initiative to address healthcare worker burnout and improve patient experiences. The AI-powered scribing tools have been implemented in over 50 clinical settings across B.C., with plans for continued expansion throughout 2024.
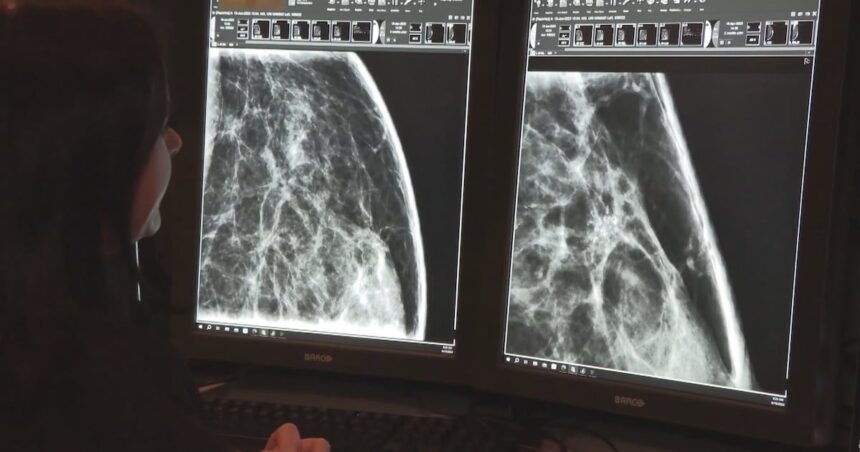
Beyond administrative efficiencies, AI technologies are making significant inroads in diagnostic medicine. At Vancouver General Hospital, radiologists are utilizing machine learning algorithms that can detect subtle abnormalities in medical imaging that might escape the human eye. “These systems don’t replace human expertise,” emphasizes Dr. Sarah Chen, head of diagnostic imaging. “Rather, they function as highly sophisticated assistants, flagging potential concerns for thorough physician review.”
The technology is particularly promising for early cancer detection. In a pilot program at B.C. Cancer, AI analysis of mammography screenings has demonstrated a 27% improvement in early-stage breast cancer identification compared to traditional screening methods alone. “Earlier diagnosis translates directly to better patient outcomes and potentially reduced treatment costs,” notes Dr. Marcus Wong, oncology research director.
Provincial health authorities have allocated $42 million toward healthcare AI infrastructure over the next three years, recognizing both the clinical benefits and potential cost savings. A recent economic analysis projects that widespread implementation could reduce administrative overhead by approximately $85 million annually while simultaneously improving care quality metrics.
However, the integration hasn’t been without challenges. Healthcare workers require substantial training to use these systems effectively, and questions about data privacy continue to shape implementation protocols. “We’re proceeding with appropriate caution,” says Health Minister Adrian Dix. “Every technology advancement must first demonstrate that it upholds our commitment to patient confidentiality and care quality.”
Patient reception has been overwhelmingly positive, with satisfaction surveys showing a 32% improvement in perceived doctor attentiveness at facilities using AI transcription. “My doctor actually looks at me now instead of typing on a computer the whole time,” remarks Vancouver resident Eleanor Chow following a recent clinic visit. “I feel heard in a way I haven’t in previous medical appointments.”
As British Columbia continues this technological transformation of its healthcare system, other provinces are taking notice. Ontario and Alberta have initiated similar pilot programs, suggesting a potential nationwide shift in how healthcare practitioners leverage AI to enhance patient care.
The question now facing healthcare administrators and policymakers extends beyond implementation logistics: In a system where human connection remains essential to healing, how do we balance technological efficiency with the fundamentally personal nature of healthcare delivery?