In the shadow of British Columbia’s acclaimed healthcare system, a troubling reality has emerged in Kelowna, where physicians are raising urgent concerns about what they describe as a “two-tiered” standard of care. Medical professionals across the Okanagan Valley are speaking out against significant regional disparities that are potentially putting patient lives at risk.
“What we’re seeing is nothing short of alarming,” says Dr. Sarah Melnyk, a veteran emergency physician at Kelowna General Hospital. “Patients here simply don’t have access to the same level of specialized care that’s readily available in Vancouver or Victoria. The disparity isn’t just inconvenient—it’s dangerous.”
The concerns center around critical gaps in specialty services, extended wait times for essential procedures, and insufficient staffing levels compared to coastal urban centers. According to data compiled by the Interior Health Physicians Association, patients in the Kelowna region wait an average of 22 weeks longer for certain specialized treatments than their counterparts in the Lower Mainland.
One particularly troubling example involves cardiac care. While patients in Vancouver experiencing certain heart conditions can access immediate intervention, Kelowna residents often face transfers to facilities hundreds of kilometers away, with critical time lost in transit. This geographic disadvantage has tangible consequences—mortality rates for specific emergency cardiac events are estimated to be 12% higher in Interior Health regions.
“We’re practicing excellent medicine with the resources we have,” explains Dr. James Chen, a cardiologist who relocated from Vancouver to Kelowna three years ago. “But the stark reality is that our patients don’t have equal access to life-saving technologies and specialists that exist elsewhere in the province. This isn’t about physician comfort—it’s about patient outcomes.”
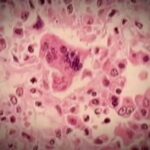
The disparity extends beyond emergency situations. Cancer patients in Kelowna face longer waits for diagnostics, treatment planning, and specialized interventions. Mental health resources remain critically understaffed compared to provincial benchmarks, with only 60% of the recommended psychiatric support available in the region.
Healthcare inequity is not a new phenomenon in Canadian healthcare, but the growing gap between urban centers and regional hubs like Kelowna represents a concerning trend. The province’s geographical challenges have historically complicated healthcare delivery, but physicians argue that technological solutions and strategic resource allocation could significantly reduce these disparities.
“We understand the financial and logistical realities,” says Dr. Melnyk. “But we cannot accept that a patient’s postal code should determine their quality of care in a universal healthcare system.”
The Interior Health Authority has acknowledged these concerns and points to recent investments in expanding Kelowna General Hospital’s capacity and specialized services. A spokesperson highlighted a $40 million allocation for enhanced diagnostic equipment and additional specialist positions approved for the coming fiscal year.
However, local physicians remain skeptical about whether these measures will adequately address the fundamental inequities. They’re calling for a comprehensive provincial strategy that ensures standardized care regardless of geography, including improved transportation networks for patients requiring specialized care, expanded telemedicine capabilities, and incentives to attract specialists to underserved regions.
As this healthcare disparity comes into sharper focus, residents throughout the Okanagan are joining physicians in advocating for equitable access. Community forums organized through local health advocacy groups have drawn unprecedented attendance, signaling growing public concern.
The situation in Kelowna raises profound questions about the future of Canadian healthcare. If a relatively well-resourced regional center like Kelowna faces such significant disparities, what does this reveal about truly remote communities across our vast nation? And more fundamentally, can we claim to have universal healthcare when the quality and accessibility of that care varies so dramatically depending on where Canadians call home?