In the crowded hallways of Newfoundland and Labrador Health Services emergency departments, the calculation behind those digital wait time displays involves more science than most patients realize. As hospitals across the province grapple with record patient volumes, understanding how the triage system actually functions has become increasingly important for those seeking urgent care.
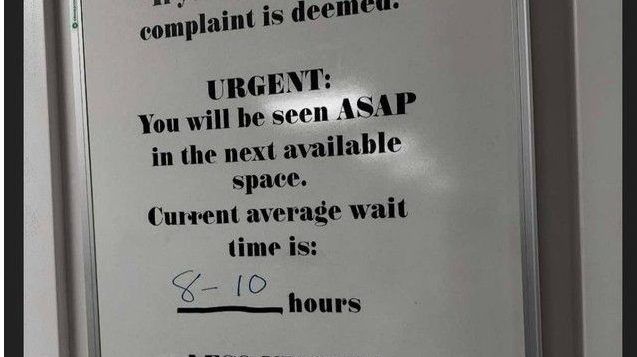
“The posted wait times represent an average of how long non-urgent patients have been waiting to see a physician,” explains Dr. Melissa Thompson, NLHS Emergency Services Director. “It’s a rolling calculation based on the previous hour of activity, not a guaranteed timeline for individual patients.”
This distinction proves crucial for managing public expectations. When arriving at an emergency department, patients undergo an initial assessment by a triage nurse who categorizes their condition according to the Canadian Triage and Acuity Scale (CTAS). This five-level system prioritizes care based on medical urgency rather than arrival time.
CTAS Level 1 patients require immediate resuscitation, while Level 5 represents non-urgent conditions that could potentially be treated at primary care clinics. The electronic displays in waiting rooms specifically reflect wait times for those classified as CTAS Level 4 or 5 – typically accounting for approximately 40% of emergency department visits according to provincial health data.
“Many people misinterpret the posted times as applying to everyone in the waiting room,” notes Sarah Jenkins, a triage nurse at St. John’s Health Sciences Centre. “In reality, we’re continuously reassessing patients and prioritizing based on clinical need, which means someone who just arrived might receive care before someone who’s been waiting longer.”
The technology behind these calculations involves specialized emergency department information systems that track patient flow, staffing levels, and capacity metrics in real-time. The NLHS recently upgraded this infrastructure as part of a $3.2 million investment in emergency services modernization.
Provincial health officials acknowledge the limitations of the current system. Internal NLHS documents obtained through information requests reveal that wait time accuracy varies considerably across different facilities, with rural emergency departments showing less reliable predictions than urban centers.
“We’re implementing a more sophisticated algorithm this coming fiscal year,” confirms Deputy Health Minister Robert Parsons. “The new system will incorporate additional variables including staffing patterns, historical usage data, and anticipated seasonal surges to provide more accurate estimates.”
For patients, experts recommend considering alternatives when appropriate. Walk-in clinics, virtual care options, and the provincial 811 healthcare line can address many non-emergency health concerns without the extended waits often experienced in emergency departments.
The challenge of emergency wait times extends beyond Newfoundland and Labrador. According to the Canadian Institute for Health Information, emergency department wait times have increased by an average of 12% nationally over the past five years, with Atlantic provinces experiencing some of the most significant increases.
As NLHS continues refining its approach to emergency care delivery, the fundamental question remains: how can our healthcare system balance transparency about wait times with the clinical reality that medical urgency, not arrival time, must always determine who receives care first?