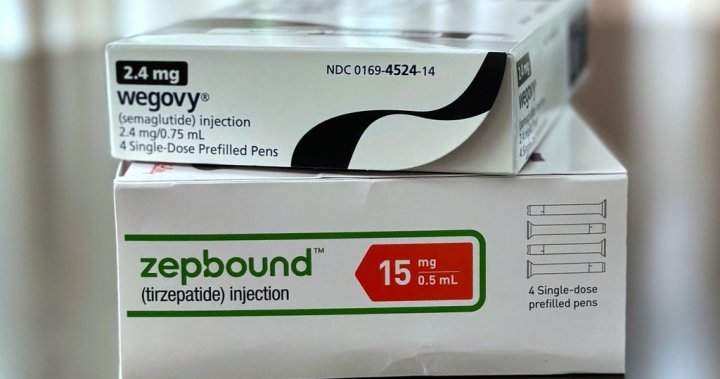
The controversial weight-loss medication that has transformed the pharmaceutical landscape may offer benefits beyond the bathroom scale. New research suggests that GLP-1 receptor agonists like Ozempic and Wegovy could significantly reduce cancer risk in patients with type 2 diabetes, potentially opening a new frontier in cancer prevention strategies.
A groundbreaking study published in JAMA Oncology examined health records of over 100,000 patients and found that individuals with type 2 diabetes who took semaglutide—the active ingredient in Ozempic—experienced a 24 percent lower risk of developing cancer compared to those using other diabetes medications.
“The implications of these findings are substantial,” says Dr. Eleanor Simmons, endocrinologist at Toronto General Hospital. “While we’ve known about the weight loss and blood sugar benefits, this potential protective effect against cancer represents an unexpected but welcome development in how we view these medications.”
The research, conducted by a multinational team of scientists across three continents, tracked patients over a five-year period. Those taking GLP-1 agonists showed particularly reduced rates of gastrointestinal, breast, and liver cancers—malignancies often associated with obesity and metabolic disorders.
Experts believe the cancer-fighting properties may stem from the drug’s anti-inflammatory effects and its ability to reduce insulin resistance—a known risk factor for certain cancers. Additionally, the significant weight loss typically experienced by patients may play a protective role by decreasing the body’s fat-stored toxins and hormones that can promote cancer growth.
However, health authorities caution against viewing these medications as cancer prevention tools just yet. “These are observational findings that show correlation, not necessarily causation,” notes Dr. Anish Kapoor, oncologist and health policy advisor. “We need randomized controlled trials specifically designed to investigate this relationship before making clinical recommendations.”
The findings come amid unprecedented demand for Ozempic and similar drugs, which has led to nationwide shortages and concerns about accessibility for diabetes patients who rely on these medications for their intended purpose.
Insurance coverage remains another hurdle. Most Canadian health plans cover GLP-1 agonists for diabetes management but not for weight loss or potential cancer prevention, creating a multi-tiered system where only those with means can access these potentially life-altering medications.
The research also highlights the increasingly blurred lines between treatments for different conditions. “We’re seeing more evidence that metabolic health impacts everything from cardiovascular disease to cancer,” explains Dr. Farrah Cheng, who specializes in metabolic disorders. “These medications are forcing us to reconsider how we categorize and treat seemingly distinct medical conditions.”
For the approximately 3.7 million Canadians living with diabetes, these findings offer cautious optimism. The possibility that their prescribed medication might provide protection against cancer adds a significant dimension to treatment decisions.
Healthcare providers and policy experts now face complex questions about how to prioritize access to these medications, especially as new applications continue to emerge. Should diabetes patients receive priority access over those seeking weight loss? How should we balance immediate medical needs against potential preventative benefits?
As research continues to evolve, one question remains central to this unfolding story: Are we witnessing the emergence of a new class of medications that transcend their original purpose, potentially reshaping how we approach multiple chronic diseases simultaneously?